Tuberculosis
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
| Chest X-ray of a patient with advanced pulmonary tuberculosis | ||
| ICD- 10 | A 15.- A 19. | |
| ICD- 9 | 010- 018 | |
| OMIM | 607948 | |
| DiseasesDB | 8515 | |
| MedlinePlus | 000077 000624 | |
| eMedicine | med/2324 emerg/618 radio/411 | |
| MeSH | C01.252.410.040.552.846 | |
Tuberculosis (abbreviated as TB for Tubercle Bacillus) is a common and deadly infectious disease caused by the bacterium Mycobacterium tuberculosis, which most commonly affects the lungs ( pulmonary TB) but can also affect the central nervous system, lymphatic system, circulatory system, genitourinary system, bones and joints.
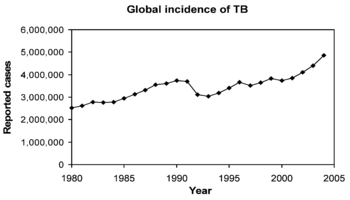
Over a half of the world's population now has the TB bacterium in their bodies and new infections are occurring at a rate of one per second. Not everyone who is infected develops the disease and asymptomatic latent TB infection is most common. However, one in ten latent infections will progress to active TB disease which, if left untreated, will kill more than half of its victims. In 2004, 14.6 million people had active TB and there were 8.9 million new cases and 1.7 million deaths, mostly in developing countries. A rising number of people in the developed world contract tuberculosis because their immune systems are compromised by immunosuppressive drugs, substance abuse, or HIV/AIDS.
The rise in HIV infection levels and the neglect of TB control programs have caused a resurgence of tuberculosis, and drug-resistant strains of TB are also emerging. The World Health Organization declared TB a global health emergency in 1993, and the Stop TB Partnership proposed a Global Plan to Stop Tuberculosis which aims to save 14 million lives between 2006 and 2015.
Other names
In the past, tuberculosis was called consumption, because it seemed to consume people from within, with a bloody cough, fever, pallor, and long relentless wasting. Other names included phthisis (Greek for consumption) and phthisis pulmonalis; scrofula, affecting the lymphatic system and resulting in swollen neck glands; tabes mesenterica, TB of the abdomen and lupus vulgaris, TB of the skin; wasting disease; white plague, because sufferers appear markedly pale; king's evil, because it was believed that a king's touch would heal scrofula; and Pott's disease of the spine and joints. Miliary TB is an archaic term that is still occasionally used, and is when the infection invades the circulatory system resulting in x-ray lesions with the appearance of millet seeds. This form of TB is now more commonly named disseminated TB.
Symptoms
In the patients where TB becomes an active disease, 75% of these cases affect the lungs, where the disease is called pulmonary TB. Symptoms include a productive, prolonged cough of more than three weeks duration, chest pain, and coughing up blood. Systemic symptoms include fever, chills, night sweats, appetite loss, weight loss, and easy fatigability.
When the infection spreads out of the lungs, extrapulmonary sites include the pleura, central nervous system in (meningitis), lymphatic system in ( scrofula of the neck), genitourinary system in urogenital tuberculosis, and bones and joints in Pott's disease of the spine. An especially serious form is disseminated, or miliary tuberculosis. Extrapulmonary forms are more common in immunosuppressed persons and in young children. Infectious pulmonary TB may co-exist with extrapulmonary TB, which is not contagious.
Bacterial species
The cause of tuberculosis, Mycobacterium tuberculosis (MTB), is a slow-growing aerobic bacterium that divides every 16 to 20 hours; this is extremely slow compared to other bacteria that have division times measured in minutes. In contrast, one of the fastest growing bacteria is a strain of E. coli that can divide roughly every 20 minutes. As MTB only has one phospholipid outer membrane, it is classified as a Gram-positive bacteria. However, if a Gram stain is performed, MTB either stains very weakly Gram-positive, or does not retain dye, due to the high lipid content of its cell wall. MTB is a small rod-like bacillus which can withstand weak disinfectants and can survive in a dry state for weeks. Normally, the bacteria can only grow within a host organism, so in vitro culture of M. tuberculosis took a long time to develop, but is now a routine laboratory procedure.
MTB is identified microscopically by its staining characteristics: it retains certain stains after being treated with acidic solution, and is thus classified as an " acid-fast bacillus" or AFB. In the most common staining technique, the Ziehl-Neelsen stain, AFB are stained a bright red which stands out clearly against a blue background. Acid-fast bacilli can also be visualized by fluorescent microscopy, and by an auramine-rhodamine stain.
The M. tuberculosis complex includes 3 other mycobacteria which can cause tuberculosis: M. bovis, M. africanum and M. microti. The first two are very rare causes of disease in immunocompetent people, and M. microti is not usually pathogenic, although it is possible that the prevalence of M. microti infections has been underestimated. Other pathogenic mycobacteria are known, such as Mycobacterium leprae, Mycobacterium avium and M. kansasii. The last two are part of the group defined as Nontuberculous mycobacteria (NTM). Nontuberculous mycobacteria are mycobacteria that are not part of the M. tuberculosis complex, and do not cause leprosy, but do cause pulmonary diseases resembling tuberculosis.
Transmission
TB is spread by aerosol droplets expelled by people with the active disease of the lungs when they cough, sneeze, speak, or spit. These infectious droplets are 0.5 to 5 µm in diameter and about 40,000 can be produced by a single sneeze. People with prolonged, frequent, or intense contact are at highest risk of becoming infected, with an estimated 22% infection rate. A person with untreated, active tuberculosis can infect 10-15 other people per year. Others at risk include those from areas where TB is common, patients immunocompromised by conditions such as HIV/AIDS, residents and employees of high-risk congregate settings, health care workers who serve high-risk clients, medically underserved, low-income populations, high-risk racial or ethnic minority populations, children exposed to adults in high-risk categories, and people who inject illicit drugs.
Transmission can only occur from people with active—not latent— TB disease. The probability of transmission from one person to another depends upon the quantity of the infectious droplets expelled by the patient, the effectiveness of ventilation, the duration of exposure, and the virulence of the Mycobacterium tuberculosis strain. The chain of transmission can therefore be broken by isolating patients with active disease and starting effective anti-tuberculous therapy.
Pathogenesis
About 90% of those infected with Mycobacterium tuberculosis have asymptomatic, latent TB infection (sometimes called LTBI), with only a 10% lifetime chance that a latent infection will progress to TB disease. However, if untreated, the death rate for these active TB cases is more than 50%.
TB infection begins when the mycobacteria reach the pulmonary alveoli, where they invade and replicate within alveolar macrophages. The primary site of infection in the lungs is called the Ghon focus. Bacteria are picked up by dendritic cells, which do not allow replication, although these cells can transport the bacilli to local ( mediastinal) lymph nodes. Further spread is through the bloodstream to the more distant tissues and organs where secondary TB lesions can develop in lung apexes, peripheral lymph nodes, kidneys, brain, and bone.
Tuberculosis is classified as one of the granulomatous inflammatory conditions. Macrophages, T lymphocytes, B lymphocytes and fibroblasts are among the cells that aggregate to form a granuloma, with lymphocytes surrounding the infected macrophages. The granuloma functions not only to prevent dissemination of the mycobacteria, but also provides a local environment for communication of cells of the immune system. Within the granuloma, T lymphocytes (CD4+) secrete cytokines such as interferon gamma, which activates macrophages to destroy the bacteria with which they are infected. T lymphocytes (CD8+) can also directly kill infected cells.
Importantly, bacteria are not always eliminated within the granuloma, but can become dormant, resulting in a latent infection. Another feature of the granulomas of human tuberculosis is the development of cell death, also called necrosis, in the centre of tubercles. To the naked eye this has the texture of soft white cheese and was termed caseous necrosis.
If TB bacteria gain entry to the bloodstream from an area of damaged tissue they spread through the body and set up many foci of infection, all appearing as tiny white tubercles in the tissues. This severe form of TB disease is most common in infants and the elderly and is called miliary tuberculosis. Patients with this disseminated TB have a fatality rate of approximately 20%, even with intensive treatment.
In many patients the infection waxes and wanes. Tissue destruction and necrosis are balanced by healing and fibrosis. Affected tissue is replaced by scarring and cavities filled with cheese-like white necrotic material. During active disease, some of these cavities are joined to the air passages bronchi and this material can be coughed up. It contains living bacteria and can therefore pass on infection. Treatment with appropriate antibiotics kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.
Diagnosis
Tuberculosis can be a difficult disease to diagnose, due mainly to the difficulty in culturing this slow-growing organism in the laboratory. A complete medical evaluation for TB must include a medical history, a chest X-ray, and a physical examination. Tuberculosis radiology is used in the diagnosis of TB. It may also include a tuberculin skin test, a serological test, microbiological smears and cultures. The interpretation of the tuberculin skin test depends upon the person's risk factors for infection and progression to TB disease, such as exposure to other cases of TB or immunosuppression.
Currently, latent infection is diagnosed in a non-immunized person by a tuberculin skin test, which yields a delayed hypersensitivity type response to purified protein derivatives of M. tuberculosis. Those immunized for TB or with past-cleared infection will respond with parallel delayed hypersensitivity to those currently in a state of infection and thus must be used with caution, particularly with regard to persons from countries where TB immunization is common. New TB tests are being developed that offer the hope of cheap, fast and more accurate TB testing. These use polymerase chain reaction detection of bacterial DNA and antibody assays to detect the release of interferon gamma in response to mycobacteria. Rapid and cheap diagnosis will be particularly valuable in the developing world.
Progression
Progression from TB infection to TB disease occurs when the TB bacilli overcome the immune system defenses and begin to multiply. In primary TB disease—1 to 5% of cases—this occurs soon after infection; in post-primary TB, secondary TB, or reactivation TB disease of dormant bacilli— 5 to 9% of cases—it occurs many years after infection. The risk of reactivation increases with immunosuppression, such as that caused by infection with HIV. In patients co-infected with M. tuberculosis and HIV, the risk of reactivation increases to 10% per year.
Other conditions that increase risk include drug injection, mainly because of the life style of IV drug users; recent TB infection or a history of inadequately treated TB; chest X-ray suggestive of previous TB, showing fibrotic lesions and nodules; diabetes mellitus; silicosis; prolonged corticosteroid therapy and other immunosuppressive therapy; head and neck cancers; hematologic and reticuloendothelial diseases, such as leukemia and Hodgkin's disease; end-stage kidney disease; intestinal bypass or gastrectomy; chronic mal-absorption syndromes; or low body weight.
Some drugs, including rheumatoid arthritis drugs that work by blocking tumor necrosis factor-alpha (an inflammation-causing cytokine), raise the risk of activating a latent infection due to the importance of this cytokine in the immune defense against TB.
Treatment
Treatment for TB uses antibiotics to kill the bacteria. The two antibiotics most commonly used are rifampicin and isoniazid. However, these treatments are more difficult than the short courses of antibiotics used to cure most bacterial infections as long periods of treatment (around 6 to 12 months) are needed to entirely eliminate mycobacteria from the body. Latent TB treatment usually uses a single antibiotic, while active TB disease is best treated with combinations of several antibiotics, to reduce the risk of the bacteria developing antibiotic resistance. People with these latent infections are treated to prevent them from progressing to active TB disease later in life. However, treatment using Rifampin and Pyrazinamide is not risk-free. The Centers for Disease Control and Prevention (CDC) notified healthcare professionals of revised recommendations against the use of rifampin plus pyrazinamide for treatment of latent tuberculosis infection, due to high rates of hospitalization and death from liver injury associated with the combined use of these drugs.
Drug resistant tuberculosis is transmitted in the same way as regular TB. Primary resistance occurs in persons who are infected with a resistant strain of TB. A patient with fully-susceptible TB develops secondary resistance (acquired resistance) during TB therapy because of inadequate treatment, not taking the prescribed regimen appropriately, or using low quality medication. Drug-resistant TB is a public health issue in many developing countries, as treatment is longer and requires more expensive drugs. Multi-drug resistant TB (MDR-TB) is defined as resistance to the two most effective first line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB (XDR-TB) is also resistant to three or more of the six classes of second-line drugs.
Prevention
TB prevention and control takes two parallel approaches. In the first, people with TB and their contacts are identified and then treated. Identification of infections often involves testing high-risk groups for TB. In the second approach, children are vaccinated to protect them from TB. Unfortunately, no vaccine is available that provides reliable protection for adults. However, in tropical areas where the incidence of atypical mycobacteria is high, exposure to nontuberculous mycobacteria gives some protection against TB.
Vaccines
Many countries use BCG vaccine as part of their TB control programs, especially for infants. This was the first vaccine for TB and developed at the Pasteur Institute in France between 1905 and 1921. However, mass vaccination with BCG did not start until after World War II. The protective efficacy of BCG for preventing serious forms of TB (e.g. meningitis) in children is greater than 80%; its protective efficacy for preventing pulmonary TB in adolescents and adults is variable, ranging from from 0 to 80%.
In South Africa, the country with the highest prevelance of TB, BCG is given to all children under the age of three. However, the effectiveness of BCG is lower in areas where mycobacteria are less prevalent, therefore BCG is not given to the entire population in these countries. In the USA, for example, BCG vaccine is not recommended except for people who meet specific criteria:
- Infants or children with negative skin-test result who are continually exposed to untreated or ineffectively treated patients or will be continually exposed to multidrug-resistant TB.
- Healthcare workers considered on an individual basis in settings in which high percentage of MDR-TB patients has been found, transmission of MDR-TB is likely, and TB control precautions have been implemented and not successful.
Several new vaccines to prevent TB infection are being developed. The first recombinant tuberculosis vaccine entered clinical trials in the United States in 2004, sponsored by the National Institute of Allergy and Infectious Diseases (NIAID). A 2005 study showed that a DNA TB vaccine given with conventional chemotherapy can accelerate the disappearance of bacteria as well as protect against re-infection in mice; it may take four to five years to be available in humans. The only TB vaccine currently in phase III trials is MVA85A, which is being trialed in South Africa by a group led by Oxford University, and is based on a genetically modified vaccinia virus. Because of the limitations of current vaccines, researchers and policymakers are promoting new economic models of vaccine development including prizes, tax incentives and advance market commitments.
Epidemiology
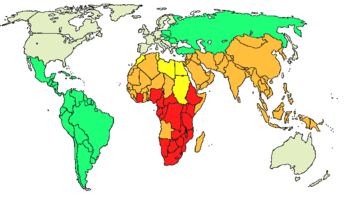
According to the World Health Organization (WHO), nearly 2 billion people—one–third of the world's population—have tuberculosis. Annually, 8 million people become ill with tuberculosis, and 2 million people die from the disease worldwide. In 2004, around 14.6 million people had active TB disease with 9 million new cases. The annual incidence rate varies from 356 per 100,000 in Africa to 41 per 100,000 in the Americas. Tuberculosis is the world's greatest infectious killer of women of reproductive age and the leading cause of death among people with HIV/AIDS.
In 2004, the country with the highest incidence of TB was South Africa, with 718 cases per 100,000 people. India has the largest number of infections, with over 1.8 million cases. In developed countries, tuberculosis is less common and is mainly an urban disease. In the United Kingdom, TB incidences range from 40 per 100,000 in London to less than 5 per 100,000 in the rural South West of England.; the national average is 13 per 100,000. The highest rates in Western Europe are in Portugal (42 per 100,000) and Spain (20 per 100,000). These rates compare with 113 per 100,000 in China and 64 per 100,000 in Brazil. In the United States, the overall tuberculosis case rate was 4.9 per 100,000 persons in 2004.
The incidence of TB varies with age. In Africa, TB primarily affects adolescents and young adults. However, in countries where TB has gone from high to low incidence, such as America, TB is mainly a disease of older people.
There are a number of known factors that make people more susceptible to TB infection: worldwide the most important of these is HIV. Co-infection with HIV is a particular problem in Sub-Saharan Africa, due to the high incidence of HIV in these countries. Smoking more than 20 cigarettes a day also increases the risk of TB by two- to four-times.
History
Tuberculosis has been present in humans since antiquity. The earliest unambiguous detection of Mycobacterium tuberculosis is in the remains of bison dated 17,000 years before the present. However, whether tuberculosis originated in cattle and then transferred to humans, or diverged from a common ancestor, is currently unclear. Skeletal remains show prehistoric humans (4000 BCE) had TB, and tubercular decay has been found in the spines of Egyptian mummies from 3000-2400 BCE. Phthisis is a Greek term for tuberculosis; around 460 BCE, Hippocrates identified phthisis as the most widespread disease of the times involving coughing up blood and fever, which was almost always fatal. Genetic studies suggest that TB was present in The Americas from about the year 100 CE.
Before the Industrial Revolution, tuberculosis may sometimes have been regarded as vampirism. When one member of a family died from it, the other members that were infected would lose their health slowly. People believed that this was caused by the original victim draining the life from the other family members. Furthermore, people who had TB exhibited symptoms similar to what people considered to be vampire traits. People with TB often have symptoms such as red, swollen eyes (which also creates a sensitivity to bright light), pale skin and coughing blood, suggesting the idea that the only way for the afflicted to replenish this loss of blood was by sucking blood.
Although it was established that the pulmonary form was associated with 'tubercles' by Dr Richard Morton in 1689, due to the variety of its symptoms, TB was not identified as a single disease until the 1820s and was not named 'tuberculosis' until 1839 by J. L. Schönlein. During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought a number of tuberculosis sufferers into the cave in the hope of curing the disease with the constant temperature and purity of the cave air: they died within a year. The first TB sanatorium opened in 1859 in Sokołowsko, Poland by Hermann Brehmer.
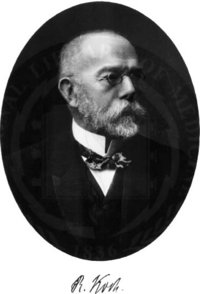
The bacillus causing tuberculosis, Mycobacterium tuberculosis, was identified and described on March 24, 1882 by Robert Koch. He received the Nobel Prize in physiology or medicine in 1905 for this discovery. Koch did not believe that bovine (cattle) and human tuberculosis were similar, which delayed the recognition of infected milk as a source of infection. Later, this source was eliminated by the pasteurization process. Koch announced a glycerine extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it 'tuberculin'. It was not effective, but was later adapted as a test for pre-symptomatic tuberculosis.
The first genuine success in immunizing against tuberculosis was developed from attenuated bovine-strain tuberculosis by Albert Calmette and Camille Guerin in 1906. It was called 'BCG' ( Bacillus of Calmette and Guerin). The BCG vaccine was first used on humans in 1921 in France, but it wasn't until after World War II that BCG received widespread acceptance in the USA, Great Britain, and Germany.
Tuberculosis, or 'consumption' as it was commonly known, caused the most widespread public concern in the 19th and early 20th centuries as an endemic disease of the urban poor. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by TB. After the establishment in the 1880s that the disease was contagious, TB was made a notifiable disease in Britain; there were campaigns to stop spitting in public places, and the infected poor were "encouraged" to enter sanatoria that resembled prisons; the sanatoria for the middle and upper classes offered excellent care and constant medical attention. Whatever the purported benefits of the fresh air and labor in the sanatoria, even under the best conditions, 50% of those who entered were dead within five years (1916).
The promotion of Christmas Seals began in Denmark during 1904 as a way to raise money for tuberculosis programs. It expanded to the United States and Canada in 1907-08 to help the National Tuberculosis Association (later called the American Lung Association).
In the United States, concern about the spread of tuberculosis played a role in the movement to prohibit public spitting except into spittoons.
In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the Medical Research Council was formed in Britain in 1913 its initial focus was tuberculosis research.
It was not until 1946 with the development of the antibiotic streptomycin that effective treatment and cure became possible. Prior to the introduction of this drug, the only treatment besides sanatoria were surgical interventions, including the pneumothorax technique—collapsing an infected lung to "rest" it and allow lesions to heal—a technique that was of little benefit and was largely discontinued by the 1950s. The emergence of multidrug-resistant TB has again introduced surgery as part of the treatment for these infections. Here, surgical removal of chest cavities will reduce the number of bacteria in the lungs, as well as increasing the exposure of the remaining bacteria to drugs in the bloodstream, and is therefore thought to increase the effectiveness of the chemotherapy.
Hope that the disease could be completely eliminated have been dashed since the rise of drug-resistant strains in the 1980s. For example, tuberculosis cases in Britain, numbering around 50,000 in 1955, had fallen to around 5,500 in 1987, but in 2000 there were over 7,000 confirmed cases. Due to the elimination of public health facilities in New York and the emergence of HIV, there was a resurgence in the late 1980s. The number of those failing to complete their course of drugs is high. NY had to cope with more than 20,000 "unnecessary" TB-patients with multidrug-resistant strains (resistant to, at least, both Rifampin and Isoniazid). The resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization in 1993.
Infection of other animals
Tuberculosis can be carried by mammals; domesticated species, such as cats and dogs, are generally free of tuberculosis, but wild animals may be carriers. In some places, regulations aiming to prevent the spread of TB restrict the ownership of novelty pets; for example, the U.S. state of California forbids the ownership of pet gerbils.
Mycobacterium bovis causes TB in cattle. An effort to eradicate bovine tuberculosis from the cattle and deer herds of New Zealand is underway. It has been found that herd infection is more likely in areas where infected vector species such as Australian brush-tailed possums come into contact with domestic livestock at farm/bush borders. Controlling the vectors through possum eradication and monitoring the level of disease in livestock herds through regular surveillance are seen as a "two-pronged" approach to ridding New Zealand of the disease.
In both the Republic of Ireland and Northern Ireland, badgers have been identified as a vector species for the transmission of bovine tuberculosis. As a result, the government in both regions has mounted an active campaign of eradication of the species in an effort to reduce the incidence of the disease. Badgers have been culled primarily by snaring and gassing. It remains a contentious issue, with proponents and opponents of the scheme citing their own studies to support their position.